The ‘admin-work’ problem is impacting clinicians across Australia. Despite over two-thirds of Australian practitioners exclusively using electronic medical records, there are still many healthcare professionals struggling to fully embrace the power of paperless systems, which results in excessive administration and workflow duplication[1&2]. These impacts are hindering practices and practitioners by causing cost, resourcing, and workflow headaches.
It is estimated Australian clinicians spend around nine hours each week on administrative duties and an additional four hours on Government paperwork, costing clinics around $15,000 per year in lost income[1]. (Based on a survey by the Australian Medical Association)
These unbillable hours spent on administration take time away from caring for patients and can put doctors under workload strain, affect work-life balance, and increase the risk of burnout.
For many specialists, catching up on clinical documentation is a key contributor to this administrative burden. We launched a Beta and Early Adopter program in 2022 to dive into the pain points doctors were experiencing regarding clinical documentation. In this program, The Magentus Practice Management Team spoke to 22 doctors and these were the common findings:
- Doctors often stay late or work on weekends to catch up on dictation
- Processes often involve receiving and reviewing transcriptions in bulk (such as from external typists), creating a build-up of work, additional stress, and delayed letter turnaround times
- Documentation was more accurate when completed close to the patient interaction
- Some use of dictation tools (microphones or software) occurred, however the ability of these tools to alleviate the above issues depended on the type of tool in use
These findings made it clear that current documentation processes were magnifying the already significant admin burden on doctors. Some doctors had sought to solve this issue with the help of dictation tools and transcription services, however these did not always resolve workflow issues.
Jump to
Benefits of using dictation software
Dictation options for your medical practice
About medical dictation software
Medical dictation software uses speech recognition technology to transcribe spoken words into text, which is why dictation software is also sometimes known as voice to text. Dictation software will usually require a period of calibration so the AI system can learn to transcribe your unique voice. Dictation software can include phone applications, desktop applications or a combination of both, and they may use compatible hardware such as USB microphones.
The benefits of using dictation software for clinical documentation
Save time and keep your work in office hours
Clinical dictation software enables healthcare professionals to capture patient data and record clinical documentation over twice as quickly as typing, with more accuracy and completeness[4].
This can result in significant time savings across the working day, reported to range between 40 minutes to 2 hours per day[1].
Completing documentation work faster means you’re more likely to finish work on time and stay on top of sending letters and results back to referrers.
Increase quality time with your patients
Dictation software uses voice commands to insert punctuation, jump to pre-defined fields, and replace keyboard controls[1]. This reduces the amount of typing and screen time required, giving healthcare professionals more quality time to listen to and interpret patient stories, so they can improve the patient experience[3].
Make your work feel more fulfilling
Around 80% of healthcare professionals see quality patient relationships as the most satisfying part of their job[1].
Unfortunately, being short-staffed and overloaded with administrative burdens can result in time spent with patients dwindling[1&2]. In fact, according to a UK study, the average time spent on patient interactions accounts for less than 13% of a clinician’s day. Whereas a staggering 50% of their working day is spent creating, reviewing and updating clinical documentation[5]. If this 50% is anywhere close to what Australian practitioners are spending on clinical documentation, then dictation software has significant potential to improve their day-to-day lives by returning the focus to patients and boosting professional satisfaction[1].
Ensure quality clinical documentation & care
Speech recognition technology supports the creation of a more complete, accurate patient record at the point of care. This improves the quality of clinical documentation, while reducing errors, missing information and workflow duplication[1&4].
Dictation not only streamlines the recording of clinical information, but also encourages practitioners to document more comprehensive patient narratives, which go beyond basic facts and capture the nuances of each patient story [1&5].
Better yet, dictation solutions can improve communication between multi-disciplinary teams by enabling faster delivery of clinical documentation. Specialists can return letters and results to referrers more rapidly which enables referrers to implement patient care sooner. This speed of delivery can improve the quality-of-care patients receive.
Dictation options for your medical practice
If you’re ready to use dictation software in your practice, we have broken down the different options available to you. If this is your first look into using dictation to aid your practice workflows, these tips will help you avoid some common pitfalls and consider what would work best for you.
1. Manual dictation
Workflow
Manual dictation (without software) has been done for decades and is still commonplace. This method involves using a physical recording device and sending the audio files to a typist or medical transcriptionist.
Considerations
- This option is usually a much longer multi-step process, requiring letters to be transcribed by specialised medical typists (which can increase costs) or sometimes administration staff in the practice. Transcriptions are usually sent back to the practitioner for review in a batch before being sent out by administrative staff, increasing the length of time it takes to return documentation to referrers.
- Medical transcriptionists can also be an expensive service, costing some practices hundreds or thousands of dollars per month.
2. Medical dictation software (e.g. Dragon Medical One)
Workflow
There are multiple desktop programs available allowing practitioners to use a USB microphone or an associated phone app to dictate directly onto their computer. When the practitioner speaks into the microphone, this will dictate straight into the desktop program – the user then usually has to copy and paste this transcription into their other software (eg email or practice management system). Dragon Medical One (DMO) by Nuance is the most popular solution in Australia and the UK that fits into this category.
Considerations
- This option saves practitioners time and can also reduce costs of typists
- Easily copy your dictation from DMO into any computer program (eg Word, Genie, Gentu)
- The limitation with this option is that it’s usually not fully integrated with your practice management software, so you still have the extra steps of copying and pasting your documentation to get it where it needs to be
3. General dictation software (non-medical)
Workflow
Dictation is used by plenty of other industries in the same way as the two options above. Your local electronics store will usually offer a range that fits into this category, but they may not include the same medical vocabulary.
Considerations
- The main limitation with general dictation software when attempting to use it for medical transcription is the lack of a medical vocabulary. This means you’ll likely have to correct a lot of words and spend a lot of time building a custom vocabulary. Clinical dictation software such as Dragon Medical One and Voice have a built-in healthcare vocabulary which provides 99% accuracy with no training required[6].
4. Clinical dictation software fully integrated with your practice management system
Workflow
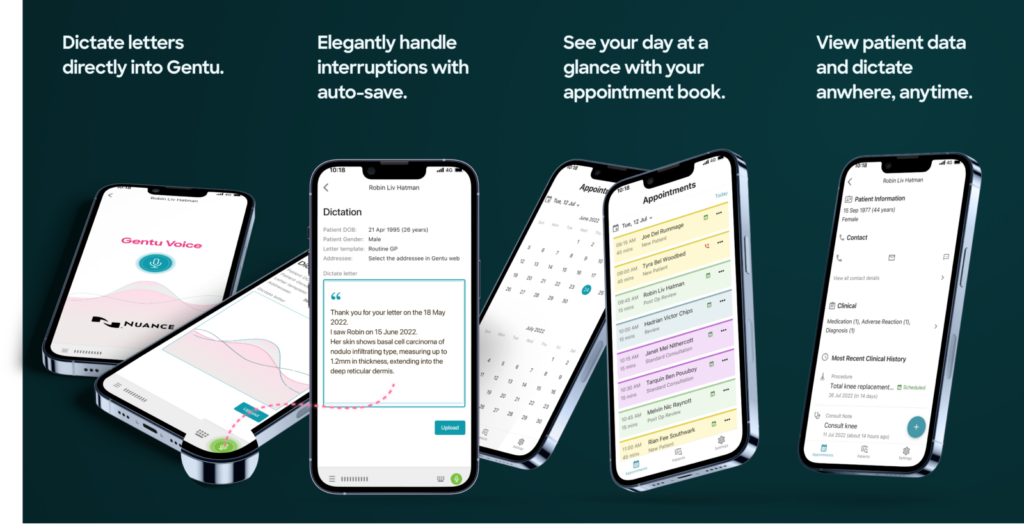
We have developed our very own medical dictation app in partnership with Nuance which is seamlessly integrated with Gentu. With Voice powered by Nuance, you will be able to dictate on your phone using the mobile app and automatically populate letters in Gentu at the tap of a button. This is a seamless experience, not possible with other medical dictation solutions which are not fully integrated with your practice management system.
This product harnesses over 20 years of Nuance’s AI learning and powerful speech recognition technology and leverages the same voice engine as Dragon Medical One.
All you need is an internet enabled smart device and some initial calibration and Voice is ready to dictate your speech and transform your workflow. Complete clinical documentation within minutes while you’re consulting with patients, immediately after appointments or on the go.
Considerations
- Voice enables Gentu users to dictate, review and upload their dictation directly to a letter in a single step
- There’s no need for external typists so you can potentially save hundreds or thousands per month on typist costs
- Voice enables you to complete documentation immediately so you can return letters to referrers faster than other modes of dictation and spend less time catching up on dictation after-hours
Find out more about Voice
If you have any questions about our medical dictation options, or general questions about improving your practice workflow, please get in touch.
References
[1] Nuance. (2021). The benefits of speech-enabling your clinical documentation [White paper]. Nuance Communications, Inc. https://www.nuance.com/en-au/healthcare/campaign/white-paper/speech-enabling-clinical-documentation.html
[2] Blackley, S. V., Huynh, J., Wang, L., Korach, Z., & Zhou, L. (2019). Speech recognition for clinical documentation from 1990 to 2018: A systematic review. Journal of the American Medical Informatics Association: JAMIA, 26(4), 324–338. https://doi.org/10.1093/jamia/ocy179
[3] Nuance Communications, Inc. (2022). AI-powered clinical documentation solutions & services. Retrieved August 14, 2022 from https://www.nuance.com/en-au/healthcare.html
[4] Vogel, M., Kaisers, W., Wassmuth, R., & Mayatepek, E. (2015). Analysis of documentation speed using web-based medical speech recognition technology: Randomized controlled trial. Journal of medical Internet research, 17(11), e5072. https://doi.org/10.2196/jmir.5072
[5] Ignetica. (2015). Accuracy & completeness of clinical documentation. Understanding the clinician, patient and economic implications in NHS England acute trusts. Ignetica ltd, [Research report]. Ignetica & Nuance. https://www.nuance.com/content/dam/nuance/en_uk/collateral/healthcare/white-paper/wp-the-clinical-documentation-challenge-uk-2015-en-uk.pdf
[6] Nuance Communications, Inc. (2022). AI powered speech recognition, a key to successful EMR implementation and adoption. Nuance. https://www.nuance.com/asset/en_au/collateral/healthcare/brochure/br-hc-save-time-and-drive-emr-adoption-with-dragon-medical-one-en-au.pdf
