In response to the ‘Workforce: recruitment, training, and retention report’, Magentus UK chief executive Robert Miller explains why we have a “collective responsibility” to empower health systems to deliver more efficient, precise and proactive care for everyone.
The workforce crisis is the greatest challenge facing the global healthcare sector today. Take for instance the UK’s Health and Social Care sector, with the latest estimates showing a shortage of nearly 12,000 hospital doctors and over 50,000 nurses and midwives across the NHS in England. Despite the huge exacerbation caused by the pandemic, the workforce crisis is not new; in 2016 the Royal College of Physicians (RCP) published a seminal report on the issue: Underfunded. Underdoctored. Overstretched.
Outlining the stark reality of the workforce problems plaguing the NHS, the RCP made three clear recommendations: Increase funding, improve the working lives of NHS staff and train more healthcare professionals. Six years later, the extent to which these proposals have been implemented remains a question for consideration.
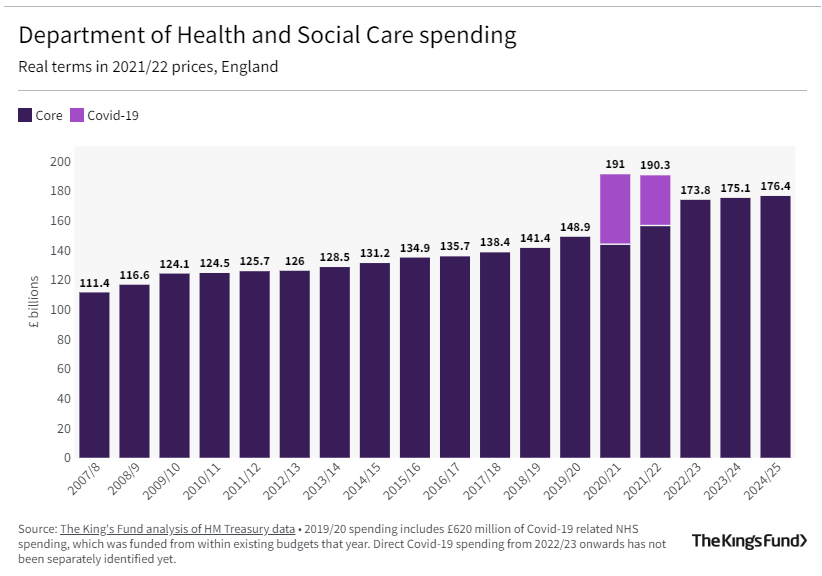
While health and social care received significant levels of extra investment in 2021, the Institute for Fiscal Studies has predicted that, in the medium term, this may not be sufficient to cover more than the extra costs associated with the pandemic. Thankfully, the numbers of NHS staff being recruited and trained has increased, but changes to flexible working conditions mean that the numbers of full time equivalent staff being recruited may be significantly less. While workforce wellbeing was improving slowly prior to the pandemic, the Health and Social Care select committee outlines a number of areas in which staff report dissatisfaction with their working conditions.
Consequently, we are now faced with an NHS that is struggling more than ever to operate under the social and economic pressures of today and a workforce leaving in droves.
The human cost: NHS staff and patients
Following COVID-19, the persistent inability to attract and retain trained healthcare professionals poses a threat to the growing treatment backlog and ever-increasing waiting lists for care. According to the 2021 Royal College of Radiologists clinical radiology census, almost 60% of radiology leaders are concerned that there are not enough diagnostic and interventional radiologists to provide safe patient care.
Staff clearly feel the same: “I care deeply about being able to care for patients without it feeling like a conveyor belt;” said Marcus Tavarez, a radiographer based in the West Midlands. “Having the time to engage and connect with them helps me to give them the best care and the best experience – that is the job that I signed up for. Working with outdated, disconnected systems and without the right resources, alongside radiology teams that have been short staffed for so long, it just isn’t possible to do that.”
A longer-term solution will clearly involve a significant strategic and explicit approach to tackle urgent vacancies and ongoing retention. However, in the short term, identifying ways to improve technical workflow efficiency and relieve front-line workers of laborious administrative tasks, is an obvious way to promote their positive mental health and headspace. Priority must be given to more interoperable digital solutions, as well as increasing collaboration between trusts.
Technology: One solution amongst many
We know that technology is not the entire solution and that funding and training matter, but technology can play its part in improving the efficiency of time, resources and costs and – most importantly – patient care. Improving workflows as well as cross and inter-organisational interoperability allows information to be shared more easily, saving precious time for the workforce and patients alike. Within clinical radiology alone, the workplace shortfall is predicted to reach 44% by 2025. To sustain a functioning healthcare system that is equipped to cope with growing recruitment and financial demands, long-standing data silos must be overcome, and remote and flexible working prioritised where possible.
The British Medical Association has made it clear that “filling in forms, dealing with correspondence, writing discharge summaries, [and] completing mandatory coding and compliance sections on computer systems” all cause significant, unnecessary bureaucracy for HCPs. Our partnership and collaboration with radiology, pathology and maternity services across the UK, has shown how consolidation, automation and increased interoperability can help to improve staff capacity and reduce the demand burden on services and healthcare professionals.
The findings of the workforce report, whilst deeply concerning, are not unsurprising. We’ve been aware of these issues for a long time now, but this report clearly and concisely sets out the true extent of the issue in the UK. These issues are also not unique to the UK either – we’re seeing the same problems unfold in health systems globally, where services are overstretched and struggling to keep pace with the delivery of healthcare expected by patients.
Clearly there are a number of important pieces of this puzzle, however technology can go some way to alleviating the challenges. COVID has forced us all to rethink so much of our lives, including the way we work and interface with other people, organisations and systems.
We are now moving away from the outdated thinking that dictates that certain tasks or roles must be carried out in specific physical locations — COVID has taught us to reconsider this perspective, with a realisation that it is possible to successfully operate remotely. Radiology is a great example where, with the right data sharing system in place, images can be reviewed, and diagnoses and recommendations made from outside the hospital walls.
What we do know is that technology has its limits, and healthcare will always require a human touch. AI and machine learning can provide us with data, but ultimately much of the time we’ll still need a specialist to review and analyse the information, and then advise on the appropriate next steps in the patient journey.
So, the question really is, how do you move the information around seamlessly across multiple organisations to allow reporting to be done anywhere by specialists?
One area in which this issue has become particularly salient is in large, rural communities where diagnostic facilities and specialists are few and far between, but people living there still require specialist advice from radiology teams.
Innovators should aim to meet health systems where they are today — by prioritising small scale, measurable changes that have a positive impact in the short term, then setting sights of the loftier aspirations for full system transformation where the benefits may take several years to be fully realised.
Collaboration across the industry will also be critical — rather than one provider solving one part of a problem, innovators should be exploring new ways to partner with other providers to help create solutions that can have a more significant impact by solving bigger problems.
Ultimately, as an industry of innovators and supporters of the NHS, we have a collective responsibility to empower health systems to deliver more efficient, precise and proactive care for everyone, by providing intelligent, collaborative and scalable solutions. By simplifying healthcare journeys and clinical workflows and putting people at the centre, we can help reduce the burden placed upon our care services.”
This piece first appeared in Health Tech World in November 2022 as “Underfunded. Underdoctored. Overstretched” – Why Health Tech is one solution among many
